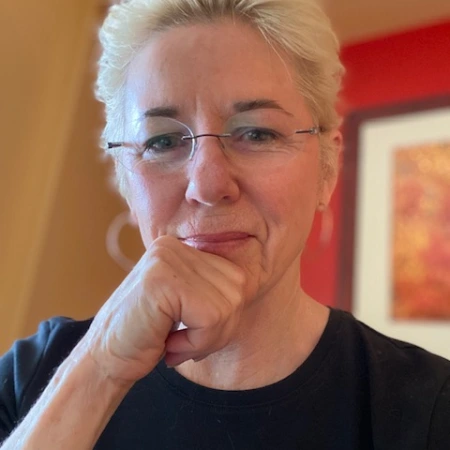
Author: Jane Ellen Stevens
publisher of ACEsTooHigh.com, long-time health/science/tech journo

This isn’t your usual article about how bad domestic violence is; it’s about a solution

To end domestic violence, heal the abusers…say those who do

2 Worth checking out: Neighborhood uses ACEs to prevent opioid deaths; burgeoning research about PACEs science
2 Worth checking out: innerBoy app a promising solution for family violence. Could Ozempic curb cravings for alcohol, shopping & gambling?
2 Worth checking out: Childhood adversity linked to health, financial problems in older adults; bill introduced to untangle poverty from child neglect
ACEsTooHigh spins off from PACEs Connection

Mayday at the Bottom of the World

Mass shootings and the news media: Catching up to the science of PACEs