Category: Community prevention programs


To end domestic violence, heal the abusers…say those who do

2 Worth checking out: Neighborhood uses ACEs to prevent opioid deaths; burgeoning research about PACEs science

There’s no mystery to what happened in Uvalde; there were many opportunities to prevent it .

To prevent mass shootings, don’t bother with motive; do a forensic ACEs investigation

PACEs champion Rebeccah Ndung’u launches trauma-informed schools in Kenya

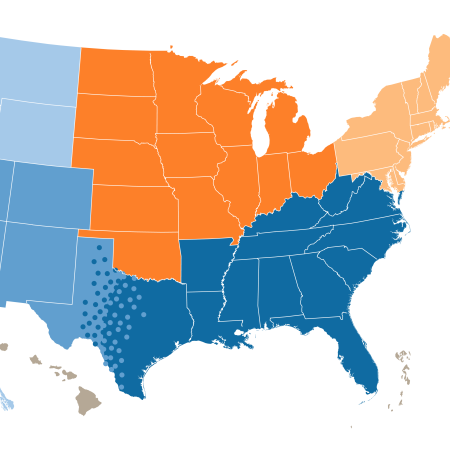
Gun violence expert says tackling underlying inequities key to prevention
Think you know something about historical trauma? PACEs Connection’s ‘Historical Trauma in America’ series promises to be an eye-opener

Lesson learned integrating ACEs science into health clinics: Staff first, THEN patients